Students
Welcome!
If you have moved to Liverpool for your studies you will be living in Liverpool for the majority of the year and so this is seen as your main place of residence. It is therefore strongly recommended that you register with a GP here in Liverpool.
You can find out about registering with us here.
If you have a health concern when you are away from Liverpool during the holidays, you will usually able to register with your local GP a temporary basis.
Click on the tabs below for useful health information.
- Homesick?
- Freshers' flu?
- Alcohol
- Cervical smears
- Diabetes
- Drugs
- Eating disorders
- Family crisis
- Glandular fever
- Medical reports/forms
- Meningitis
- Mental Health
- Mumps
- Prescription charges
- Sexual health
- Sports injuries
- Weight management
- Sick notes
Homesick?
For many this is the first time away from the family. So much is unfamiliar that the feeling quickly creeps in that you’d be better off at home. The first thing to say is that this is very normal! Most of us have been through this, and it most cases this settles down in the first few months.
Here are some tips that might help:
- Remind yourself that it’s natural to miss your old life as it’s more cosy and familiar.
- Talk to someone about how you’re feeling, such as new friends, family or welfare officers.
- Make the most of social opportunities, but also remember it’s ok not take part in everything. Most of us need a bit of space now and again, and you’ll be more resilient if you have some ‘chill out’ time.
- Establish a balance between study, work and leisure.
- Establish a routine.
- Remember to eat well, sleep and consider exercise.
- If it is getting worse, seek help from a doctor, nurse or counselling services
If you feel like you’re struggling, and have feelings of anxiety or feeling low that won’t go away, then it may be that you need some extra help. NHS choices has some useful advice on managing stress, anxiety and depression, and you might want to consider making an appointment to see a nurse or doctor here at the practice.
The Universities also all have counselling services. Check under the ‘Mental Health’ tab for more information. You can self refer, without necessarily seeing a doctor first.
‘Fresher’s Flu’
There isn’t an actual medical condition called ‘Fresher’s Flu’, but anecdotally students are more prone to catching a virus that lays them low in the first few months of university life. This isn’t too surprising, as students gather from all parts of the country and the rest of the world, sharing coughs and colds that our immune systems aren’t used to. These viruses also spread more easily because students are often gathered in large numbers, in close proximity, for example in lecture theatres and halls of residence.
Added to this mix is often poor diet, less sleep, alcohol, and other drugs that make us more vulnerable to illness.
You can reduce your risk of getting ill by:
- Drinking plenty of water
- Getting fresh air and exercise
- Eating well.
- Avoiding too much alcohol
- Getting more sleep. We know that part of the fun of university is the late nights and going out, but by trying to space these out with some more relaxed night in you’ll be making yourself much more resilient against illness.
What to do when you’re ill
NHS choices has some useful advice about managing coughs and colds. If you’re still not sure, you can call us for a telephone consultation, or make an appointment with the nurse.
Alcohol
There is a wide variation in people’s approach to drinking alcohol, and it’s worth considering which category will describe you:
-Non-drinker
-Drinking alcohol with safe limits
-Harmful binge drinking (episodic drinking, but above recommended limits)
-Harmful ‘chronic’ alcohol use (regularly drinking above recommended limits)
It is a good idea to consider a safe approach to alcohol early on in your student life. This means you can enjoy your social life without risking the adverse effects. Here at the student health centre, we often see people suffering from the consequences of the latter two categories, including A+E attendances, liver damage, gastritis, mental health issues, sexual vulnerability, weight gain, addiction, and adversely affecting their degree prospects. These issues can be avoided by making yourself aware of safe limits, and planning in advance to keep within these limits.
What are the recommended safe limits?
The current UK guidelines advise limiting alcohol intake to 14 units a week for women and men. This is equivalent to drinking no more than 6 pints of average-strength beer (4% ABV) or 7 medium-sized glasses of wine (175ml, 12% ABV) a week.
Remember, these are maximum recommended limits, not targets!
In general, the more you drink above the safe limits, the more harmful to your health alcohol is likely to be. And remember, binge drinking can be harmful even though the weekly total may not seem too high. Binge drinking is generally defined as consuming eight or more units in a single session for men and six or more for women.
The DrinkAware website have developed a useful unit and calorie calculator– why not try it for yourself?
You can find some useful tips on cutting down your alcohol intake here on the change4life website.
If you think you need further help with cutting own alcohol you can:
-Make a GP or nurse appointment
-Book to see our health trainer
-Contact the Liverpool Community Alcohol Service.
Cervical Smears
All women aged between 25 and 64 are invited for cervical screening. Women aged between 25 and 49 are invited for testing every three years, and women aged between 50 and 64 are invited every five years.
Being screened regularly means that any abnormal changes in the cells of the cervix can be identified at an early stage and, if necessary, treated to stop cancer developing.
More information can be found here.
Why don’t people under 25 have a smear?
We frequently get asked this, which is a very reasonable question, especially as there are occasionally high profile and tragic deaths from cervical cancer in women under 25 years of age.
However, there are good reasons for cervical smears not being done in women under 25. In fact, it may cause more harm than good.
However, it is very important that If you have symptoms such as bleeding between periods or after sex you consult your GP straight away.
Starting University is an exciting time of life, and if you have diabetes we want to enable you to make this transition and enjoy your time here, whilst reducing the risks of your diabetes causing any complications.
With this in mind, we are very fortunate at Brownlow Health to have a Diabetes Nurse Consultant, Peta Navein, on our team. This level of specialist nursing support has previously only been available in hospital diabetes clinics.
On 27th November 2015 Brownlow Health was named “Diabetes Team of the Year” at the UK GP awards for this work in improving diabetes care among student in Liverpool.
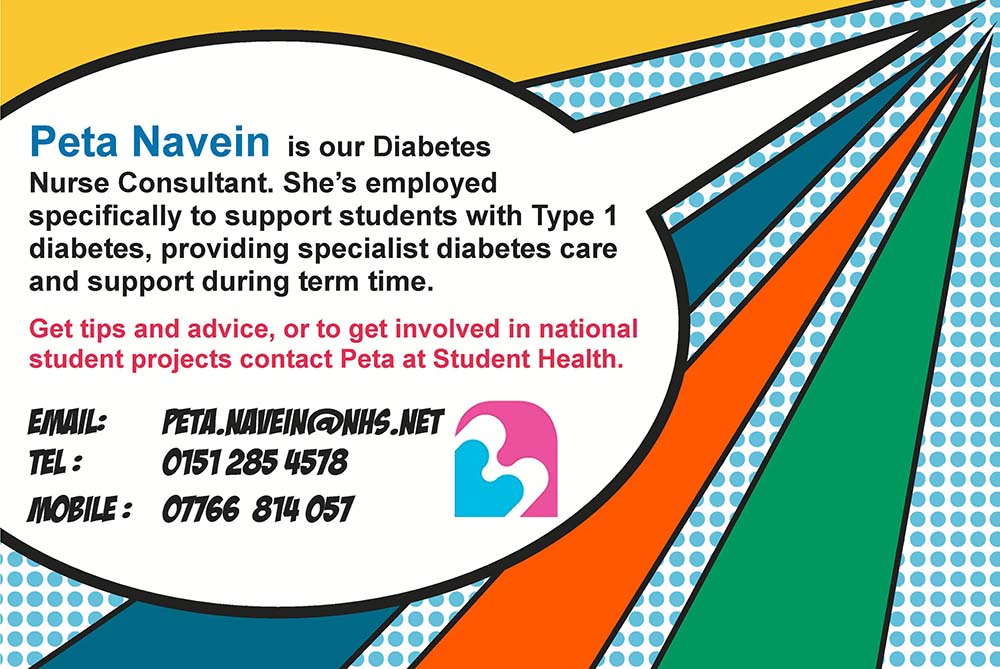
Pete Navein, diabetes nurse, contact details poster
We know that many students prefer to keep their diabetes reviews with the home Consultants and see them when they go home in the holidays. However this can also mean that students do not have access to specialist advice whilst in Liverpool if things are not going so well. We therefore encourage our newly registered students with diabetes to make early contact with Peta during the first few weeks of the term. You can do this by asking for an appointment via reception. Peta will then liaise with your home team and agree with each student what support they need during term time. She will provide you with her contact details so you can easily get advice, as well as advising on how to get medical advice for if she is not available.
In the mean time, you might find it helpful to read the useful ‘Starting University with Diabetes’ leaflet from Diabetes UK.
We’ve also listed a more extensive list of useful diabetes leaflets in our resources section.
Drugs & Alcohol
Some useful links
Addaction, a UK based drug and alcohol treatment charity. Useful online information, and details of local services.
Calories in Alcohol. The ‘Fewer Units. Fewer Calories’ campaign.
Drink Aware– Help, facts and advice about alcohol.
Sanctuary– Support for substance misusers, their families and their carers.
Strange Molecules – the essential facts on ‘legal highs’, plus help and advice
Talk to Frank. Friendly, confidential drugs advice.
Eating Disorders
Eating disorders are illnesses that stem from both emotional and psychological distress and result in an obsessive relationship with food in terms of over or under eating. Having the ability to control the amount and type of food consumed makes sufferers believe they are coping with their problems and offers a way to block out painful feelings.
If you are concerned, you should book an appointment with any GP at the practice.
Anorexia Nervosa
A person with anorexia nervosa deliberately loses weight. The weight loss may become severe and life threatening. Treatment includes cognitive behavioural therapy, if appropriate, sometimes medication and self help measures.
Anorexia is a serious illness which affects all sorts of people. Although it is regarded as a fairly recent illness, in fact anorexia has been known about since medieval times. However, it is becoming more common all over the world.
For more information see this information leaflet from Patient.co.uk.
Bulimia Nervosa
People with bulimia nervosa have bouts of binge eating. This is followed by self-induced vomiting or other measures to counteract the excessive food intake.
Bulima is a condition where you think a lot about your body weight and shape. It affects your ability to have a ‘normal’ eating pattern. In bulimia you are most likely to be normal weight or above. For more information see this information leaflet from Patient.co.uk.
Family crisis
Hope Support offers support for young people when a close family member is diagnosed with a life-threatening illness. There is a section specifically for students on their website, including the option of online one to one support.
Glandular Fever
Also known as the ‘kissing disease’ glandular fever is caused by an infectious virus which is passed on by saliva and from coughs and sneezes. Glandular fever causes a flu like illness with temperature, headache, sore throat and swollen glands and can cause a tiredness lasting for some time after first onset.
Glands may swell in the armpits and groin, and diagnosis is confirmed by a blood test. There is no treatment for glandular fever but it can be helped by drinking plenty of water, eating healthily and keeping a good sleep pattern with plenty of rest.
Click here for information about fees for reports and letters.
What is meningitis?
Meningitis is a serious disease in which there is inflammation of the membranes (meninges) surrounding your brain and spinal cord, caused by viral or bacterial infection, and marked by intense headache and fever, sensitivity to light, and muscular rigidity.
Many people unfortunately still believe that meningitis only affects babies and young children. This is not the case. Meningitis can affect anyone, of any age, at any time; it can strike quickly and kill within hours.
Students are considered to be a higher risk group for meningitis, and you should familiarise yourself with the signs and symptoms, so you can watch out for them in yourself and your friends. (It is sadly not uncommon for there to be deaths of students from meningitis each year in Liverpool.)
“Meningitis now” have developed a smart phone app. Why not download it now so you always have the signs and symptoms handy to refer to?
Vaccination for students
A new vaccination programme has been launched (September 2015) for all 17 and 18 year olds to be vaccinated against the A,C,W and Y strains of meningococcus. This doesn’t cover all causes of meningitis, but is an important step in reducing incidences of this deadly disease among students.
New university and college entrants (freshers) up to the age of 25 are also eligible for vaccination. Ideally you should have this from your GP before starting University, but there will also be catch up sessions for those who have missed it, or you can simply book with the nurse to request this in a regular appointment.
Mental Health
All the universities in Liverpool have counselling services for their students:
University of Liverpool Counselling Service
Liverpool John Moores University Counselling Service
Hope University Counselling Service
Other services
Big White Wall – Online support for University of Liverpool students
Nightline– a night time listening and advice service run by the University of Liverpool Guild of Students.
Alternatively you can seek counselling privately. The Counselling Directory is a useful resource for finding a therapist to suit your needs.
Self Help
As well as the tips below, there is some fantastic self help information on the Merseycare website.
Stress
Recent surveys have shown that students are experiencing increasingly severe emotional problems. The number of students seeking help is rising faster than ever.
A little bit of stress is good for the body but when it builds up we need to learn how to deal with it.
View stress as a warning that some aspects of your life might need changing. Main offenders include money worries, work, study, relationships and lifestyle.
Stress busters
Relaxation
Muscular relaxation exercises and deep breathing are two common techniques to help people to relax and combat symptoms of anxiety. For further information on relaxation exercises visit Patient.co.uk.
Exercise
Choose the right exercise and you’ll feel both energised and relaxed. In general yoga and Tai Chi are excellent for reinstalling calm by focussing on breathing and centering the mind.
Physical exercise will reduce stress by using up adrenalin and can relax muscles.
Eating a healthy diet
Processed foods, too much salt, sugar, alcohol and caffeine can all drain energy.
Get enough sleep
Regulate your sleeping hours by going to bed and waking up within a time slot of 1 to 2 hours
De-clutter your life
Just say ‘no’ to demanding colleagues, friends and family. You know how much you can cope with, so pick the important stuff. Prioritising lists can often help you decide what really needs to be done and what can wait.
Laugh!
Research shows that not only does this improve mood, it relieves stress and boosts the immune system.
Depression
Depression is common. Symptoms can affect day to day life and can become very distressing. Treatments include counselling and antidepressant medicines. Treatment takes time to work but has high levels of success. Some people have recurring episodes of depression and require long term treatment to keep symptoms away.
For an information leaflet visit Patient.co.uk.
Anxiety Disorders
Most people feel anxious from time to time. However, anxiety can become abnormal if it interferes with your day to day activities. Anxiety is a symptom of various disorders which are discussed in this information leaflet. They can often be treated. Treatments include counselling and medication.
Mumps
What is Mumps?
Mumps is an infection caused by a type of virus called a paramyxovirus. It is very contagious and spread in saliva, the same way as a cold or flu. This means it can be caught from an infected person coughing, sneezing, etc. Or, from touching infected objects, for example, door handles. Mumps infection is less common since the introduction of the measles, mumps and rubella (MMR) vaccine in the UK. (See separate leaflet called ‘MMR Immunisation’ for more information.) Mumps infection is now most common in children who have not received the vaccine.
What are the usual symptoms of mumps?
- Swelling and pain of one or both parotid glands are the usual main symptoms. The parotid glands are the main salivary glands. They are just below the ears and you cannot normally see or feel them. The salivary glands make saliva which drains into the mouth.
- The mouth may feel dry.
- Chewing or swallowing may feel sore.
- Fever (high temperature), headache, feeling tired and being off food may develop for a few days.
- Mild abdominal (tummy) pain may occur.
The swelling of the parotid glands usually lasts 4-8 days. Mumps is normally a mild illness, but complications sometimes occur. This is why immunisation is important.
There may be no symptoms, or only very minor ones. It is thought that about 3 in 10 people who contract the mumps virus have no symptoms. Rarely, complications alone occur without the usual symptoms occurring first. The immune system makes antibodies during the infection. These clear the virus and then provide lifelong immunity. It is therefore very rare to have more than one episode of mumps.
What are the possible complications of mumps?
The outlook for young children with mumps is very good. Teenagers and adults with mumps are more likely to develop complications, which may include one (or more) of the following:
- The testes (testicles) are sometimes affected. One testis may become inflamed, swollen, and painful for about a week. This is uncommon in young children. However, about 1 in 4 males who get mumps over the age of 12 develops a painful swollen testis. Occasionally, both testes are affected. In very rare cases this may cause infertility.
- Brain inflammation (encephalitis or meningitis) is an uncommon complication. It typically causes drowsiness, headache, stiff neck, wanting to keep out of the light, and vomiting. Although alarming, meningitis caused by the mumps virus usually clears after a few days without any long-term problems.
- Hearing loss can occur in around one in twenty people with mumps. This is usually only transient and usually improves with time. Very rarely, mumps can cause permanent deafness.
- Inflammation of the pancreas, heart, and other organs are rare complications.
- If you develop mumps in the first 12-16 weeks of a pregnancy, it may increase the risk of miscarriage. (However, the mumps virus is not thought to cause malformations or defects in an unborn baby.)
How is mumps diagnosed?
Mumps is most commonly diagnosed by your symptoms and the type of glands that are enlarged in your body. However, some people have a swab taken from their mouth to obtain some saliva. This is sent to the laboratory to confirm the diagnosis.
What is the treatment for mumps?
There is no drug that kills the mumps virus. TFor most people, mumps improves over a week with no long-term problems.
Treatment aims to ease symptoms until the body’s immune system clears the virus.
- You do not need any treatment if symptoms are mild
- Paracetamol or ibuprofen can be beneficial to ease fever and pain.
- Give children lots to drink, particularly if they have a fever. Fruit juice may stimulate the parotid gland to make more saliva, and cause more pain. Water is best if this occurs.
- A warm flannel held against a painful parotid gland is soothing.
When to seek medical help?
Most people are back to normal within 7-10 days. Seek medical help if you suspect that a complication is developing (described above).
Should people with mumps keep away from others?
Yes. Mumps is very infectious. It takes 14-21 days to develop symptoms after being infected. Affected people are infectious from about six days before, until about five days after, a parotid gland begins to swell. People with mumps should therefore stay off school, nursery, college or work and avoid other people as much as possible. This is as soon as mumps is suspected and for five days from the onset of parotid gland swelling.
Mumps immunisation
An effective vaccine to prevent mumps is available. It is part of the MMR vaccine. This is routinely offered to all children aged 12-15 months in the UK. A second dose is offered as part of the routine pre-school booster programme at four years of age. The routine MMR vaccinations were only introduced in 1988, so some students may have missed this, and others may not have been immunised for other reasons. If you are not sure, you should see the nurse. If in dout, you will be given a booster. Having an extra dose causes no harm. Also, it does not do any harm if you have had mumps in the past and then have the MMR vaccine.
Immunisation gives very good protection, and so mumps is now rare in the UK. However, in recent years there has been an increase in the number of cases of mumps, usually seen in people who have not been immunised with MMR.
For further information visit: NHS Choices website
All students are entitled to free prescriptions up to and including the age of 18. After that, statutory prescription prices will then apply (currently £9 per prescription). However, some people may still be entitled to free prescriptions based on low income grounds- reception can give you an HC1 form if you want to apply for this.
Sexual Health Services
At Brownlow Health we provide comprehensive and confidential sexual health and contraceptive services.
Simply ask for one of the nurse appointments via reception.
Our services include contraceptive implant and coil insertion, for which there is a dedicated clinic at Ropewalks practice on Monday evenings, 5-7pm. To access this, please ask your doctor or nurse, or at reception, and the relevant nurse will be in touch with you to explain the procedure and arrange your appointment.
Ropewalks site: Monday evenings 5-7pm.
Student Health: Tuesdays 10-12
Contraceptive Services
We are able to advise on and deliver the full range of contraceptive services including
- Contracecptive Implants – insertion and removal
- Intra uterine contraceptive devices – Copper and Mirena coils
- Contraceptive injection
- Oral Contraception – combined and Progesterone only pills
- Condoms
- Contraceptive rings and patches
This useful video from NHS choices outlines all of the options
Screening for Sexually Transmitted Infections (STIs)
We are able to screen and arrange treatment for a range of conditions
- Chlamydia and Gonorrhoea- swab or urine sample
- Trichomonas – swab
- Genital warts
- Genital herpes
- Hepatitis B and C – blood test
- HIV – blood test
- Syphilis – bloood test
Additional Swabs
- Candida (Thrush)
- Bacterial vaginosis
Cervical Smears
All women aged between 25 and 64 are invited for cervical screening. Women aged between 25 and 49 are invited for testing every three years, and women aged between 50 and 64 are invited every five years.
Being screened regularly means that any abnormal changes in the cells of the cervix can be identified at an early stage and, if necessary, treated to stop cancer developing.
More information can be found here.
Useful Links
Sexual Health Liverpool. Advice, support, and alternative local services.
Rape and Sexual Abuse Centre for Women in MerseysideHelpline: 0151 666 1392
Safe place Merseyside
Marie Stopes
Bpas
Sports Injury Clinic
(University of Liverpool Students only)
If you are a member of the University of Liverpool Athletics Union you can access to the Sports Injuries Clinic, run by experienced sports physiotherapists. The clinic, located in the Student Health Centre, is open during term time on Mondays, Tuesdays & Wednesdays from 5.15pm to 7.30pm
To book an appointment, please bring your AU membership card /AU number to the Student Health reception.
Students are asked to arrive for their first session 10 minutes before the appointment time for the process of information gathering. Please bring your valid AU membership card with you.
Note: AU members do not have to be registered with Student Health to access this service.
Weight management
If you are concerned about your weight please book an appointment with a doctor, a nurse or our health trainer to see how we can help you.
The causes and solutions for weight gain can be complex and there is a considerable amount of dodgy information and even dodgier medications that we would recommend you to avoid.
As well as excluding medical causes, and supporting you, there are free local services that we can refer you to, if appropriate, to help you to identify the right pathway for you.
Six of our GPs specialise in weight management and are part of the team for the NHS Liverpool specialist community based service with aintree hospital known as ‘Aintree LOSS’ providing specialist dietetic advice, physiotherapy, occupational therapy, psychology and medical management and assessment for weight loss surgery.
In order to access the ‘Aintree LOSS’ service, you must meet the following criteria:
Aged at least 18 years
BMI >40 with or without obesity related co morbidities
BMI > 35 with at least one obesity related co morbidity
Sick notes
Most educational establishments have a sickness absence policy stating that you can self certify for a short period without needing a doctor’s note.
The Sickness Absence Policy for the University of Liverpool states that a self certificate is valid for absences of up to 5 days (with a few exceptions). Most universities will have a similar policy.
If you do need a doctors note, this is considered as non-NHS work and therefore there will be a charge. A list of our current charges can be found here.
Please note that the University of Liverpool will no longer be covering this charge for their students, and the student will therefore be required to pay this directly to the practice if a note is needed.
You may notice that our online consultation provider has recently changed from E-consult to Blinx Healthcare, however this has not impacted how we process your requests. Please continue to submit online consultations using our new platform and your query will be reviewed the same day.
CONTACT US ONLINE
Admin requests, sick notes, booking certain appointments, and more.
PRESCRIPTION REQUESTS
Find out how to order repeat prescriptions online.
REGISTER
Register as a patient with the practice.